Normal insulin release
The pancreas is an organ in the upper abdomen that releases insulin in two ways:
- In a steady manner continuously called basal insulin. Basal insulin helps our body use glucose to carry out vital ‘background’ functions (circulation, respiration, brain activity, etc.)
- In rapid surges around mealtime, to prevent blood glucose (BG) from rising excessively. This surge allows our body to use glucose from ingested food to make energy for voluntary functions like muscle activity (our movements).
What is an insulin pump?
- Small computerized insulin delivery device
- Delivers insulin in a manner similar to how the normal pancreas delivers in a non-diabetic individual.
Insulin pump therapy is part of the wave of new advances in medical technology that has revolutionized the management of diabetes.
Insulin pumps deliver rapid-acting insulin in a manner that closely mimics the natural insulin delivery by the pancreas, allowing a more precise insulin delivery to match patients’ unique needs based on their size, activity, and food intake. Many insulin pumps are connected to continuous glucose monitoring systems (CGMS). The CGMS may be ‘integrated’ with the insulin pump so that insulin delivery can be adjusted based on glucose level using specialized algorithms and artificial intelligence. This feature offers advantages such as:
- Automatically adjust insulin delivery based on CGM glucose reading.
- Adjust insulin delivery based on ‘predicted’ BG trends.
- Deliver automatic correction dose of insulin if glucose levels are high.
- Adjust insulin delivery settings for activity, sleep, stress, etc.
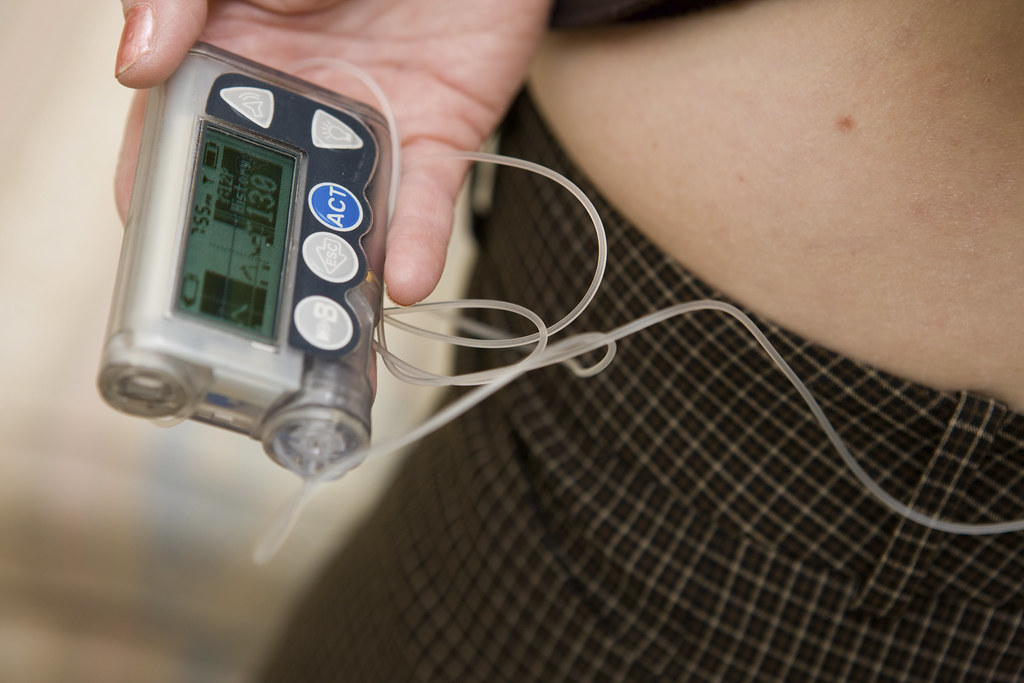
What are the parts of an insulin pump?
- Pump
- Reservoir
- Tubing
- Cannula
- Insulin
- Some pumps are connected to & communicate with sensors /CGMS.
The insulin pump itself is a small, computerized insulin delivery device that uses only rapid–acting insulin. The reservoir is the part of the insulin pump that contains the insulin for delivery. The reservoir is connected to the tubing that moves the insulin from the reservoir to the site.
The site is the point where the insulin pump is connected to your body. An insulin pump is inserted in the same places that are used for insulin administration by syringe: the abdomen, arms, buttocks, and thighs. A needle is inserted at the pump site, but then the needle is removed to leave a soft, pliable catheter in your body (the cannula). The pump site is usually changed every 2-3 days to prevent infections or build- up of scar tissue that would interfere with insulin absorption.
What can I do to prepare for an insulin pump?
- To best prepare for insulin pump therapy, you should be competent in basic diabetes management and be an active participant in your diabetes care.
- You should have realistic expectations of insulin pump therapy and be motivated to learn new skills. The insulin pump is not a magic cure for diabetes and does require the operator to check their blood sugar multiple times daily (or use a CGMS – Continuous Glucose Monitoring System) as well as count carbohydrate grams at each meal.
- Review ketone testing by blood or urine and have ketone testing supplies available before you start the insulin pump.
- Learn how to count carbohydrates and practice your carb counting skills before starting on an insulin pump.
- Have a written plan for ‘sick day’ management of your BG (with the help of your diabetes educator or your health care provider)
- Understand what to do if you have low BG (hypoglycemia)
- Have a backup plan in case the pump stops working (uncommon)
What are the key settings for the insulin pump?
- Basal rate
- Bolus for Carbs(Insulin to carb ratio)
- Bolus for Correction (Insulin Sensitivity Factor or ISF)
- Active insulin time
- Max Bolus
- Temporary Basal Rate
Like the pancreas, an insulin pump only uses one rapid-acting insulin that is delivered in two different ways. Both continuously (basal insulin) to carry out vital bodily functions, and in surges around mealtime to prevent blood glucose levels from spiking.
The insulin to carb ratio (ICR) is the grams of carbohydrate that are covered by 1 unit of rapid-acting insulin (the correct ratio will deliver the exact amount of insulin as you eat, so your BG will not rise excessively after you have eaten)
The Insulin Sensitivity Factor (ISF) or Correction Factor is the number of points that your BG is expected to drop with 1 unit of insulin.
The target blood sugar is the blood sugar value that your pump is trying to obtain with the correction. The pump’s bolus calculator calculates your bonus dose by using these factors, along with the blood sugar value and the carbohydrate amount you enter into the pump.
An insulin pump is can administer insulin doses in fractions of a unit, allowing the pump to fine-tune the basal and bolus amount to your insulin needs.
All insulin pumps have Max Basal and Max Bolus settings. These maximums serve to limit the amount of insulin given in either a basal or bolus dose to prevent unwanted low blood sugars.
The Temporary Basal Rate allows the pump’s basal rate to be increased or decreased for a limited time. This allows the basal rate to be decreased during exercise to prevent a low blood sugar, or increased to compensate for the rise in blood sugar during illness. Typically, you can set this Temporary Basal Rate for 12-24 h at a time and most commonly as a percentage above or below the normal basal rate.
Bolus insulin doses can also be delivered at various speeds and timings to better correspond with the food digestion and BG changes.
The computer in an insulin pump also utilizes Active Insulin Time or Insulin On Board settings to track the amount of insulin that remains active in your body after a bolus insulin dose is given. This prevents stacking of insulin doses too close together which could result in low blood sugars.
Who should consider an insulin pump and why?
An insulin pump is a good choice for many patients with diabetes. These patients include:
- People who are comfortable with technology
- Patients with an active lifestyle
- Patients with variable meal timings and type of food they consume.
- Patients with frequent low BG
- Pregnant patients
- Patients who have variable food absorption (e.g. gastroparesis)
Even though pumps are essentially safe, they are not perfect. Insulin pumps are machines that can break. Tubing and sites can get pulled out or kinked. Since insulin pumps only use rapid-acting insulin, any interruption of insulin that lasts more than 1 hour puts the patient at risk of high blood sugar and high blood ketoneswhich may develop into diabetic ketoacidosis (DKA). The patient should therefore wear their insulin pump all the time.
Site infectionsandscar tissue development may occur. Fortunately, these problems are rare events and safeguards have been developed to monitor and alert you to these problems. Frequent blood sugar monitoring and/or the use of a continuous glucose monitoring device, also helps the pump wearer to promptly identify and address any pump problems should they arise.
Table 1 shows the positives (advantages) and negatives (disadvantages) of insulin pumps.
| POSITIVES | NEGATIVES |
| · May decrease the insulin required by 20-25% | · Pumps are machines and can malfunction |
| · Able to make smaller dose changes in fractions of a unit | · Pump must remain attached consistently. Cannot be off the pump for more than 1 hour |
| · Only uses one type of insulin (Rapid-acting insulin). Less expensive to use only one type of insulin | · May develop ketones if the pump is turned off for more than one hour, or the site is kinked, or if the pump site is not changed. |
| · Able to correct blood sugar when necessary | · Must bolus for all meals and snacks, and to correct blood sugar |
Most insurance plans cover insulin pump therapy. Medicare only covers insulin pumps for those with type 1 diabetes and some patients with type 2 diabetes.
Insulin pumps are made by different companies. The preferred insulin pumps in the US include Medtronic, Omnipod, and T-slim. Take time to choose your insulin pump. Study their websites. You can get more information on insulin pump therapy from your diabetes healthcare provider, diabetes educator, and certified pump trainer. Once you have decided which pump matches your needs, your healthcare provider can help order it.
INSULIN PUMP AND SENSOR WEB SITES:
www.dexcom.com Dexcom CGMS
www.medtronic.com Medtronic insulin pumps
www.myomnipod.com Omnipod Insulin Pumps
www.Tandemdiabetes.com Tandem Insulin Pumps
www.freestylelibre.us Freestyle libre CGMS
.
.
Post Disclaimer
We are not your healthcare provider, and your use of this website does not establish a patient-client relationship. All the information contained on this website is for informational purposes only. No material on this site is intended to be a substitute for professional medical advice (diagnosis, treatment, testing or nutritional information). Always seek the advice of your physician or qualified healthcare provider with any questions you may have regarding medical or health-related conditions or treatment. Your healthcare provider knows your condition or situation well and can give you specific advice which would be appropriate for your condition/situation. Your healthcare provider can also guide you more accurately about injection techniques, dietary interventions and the use of medical technology that is most pertinent and suitable for you. Please do not disregard professional medical advice or delay in seeking it because of something you may have read on this website.